Ideas by Bridgeable
Designing patient-centric self-monitoring solutions to reduce rehospitalizations
Author
- Bridgeable
Many complex diseases require patients to self-monitor their symptoms at home in order to avoid serious complications (e.g., blood glucose testing for diabetes, blood pressure monitoring for cardiovascular disease).
Modern self-monitoring services have complex requirements and cannot be designed in a vacuum. Bringing positive change to patients’ lives requires that the complexities of hospital operations, patient behavior, and 21st century healthcare be taken into account.
In this article, we highlight an exploratory project that focused on the self-monitoring experience for patients with heart failure. We demonstrate how Bridgeable’s approach can improve the current state of the patient experience and ultimately reduce the likelihood of hospital readmission while considering the broader needs of caregivers and frontline healthcare providers.

Applying a Human-Centric Lens to an Existing Challenge
Understand the patient’s needs
The design of a modern self-monitoring service must take into consideration the fact that most patients have comorbidities and must work to balance the requirements of living with multiple chronic diseases.
Weigh the benefits against various costs
The design of a self-monitoring service needs to weigh a variety of often-ignored costs (e.g., dedicated staff, investment in new technologies) against potential benefits (e.g., reduction in expensive hospital readmissions).
Consider how patient behavior affects outcomes
The design of a self-monitoring service must consider all possible patient behaviors that might have a positive or negative impact on adherence. Design elements that both enhance patient motivation and recognize patient attitudes towards lifestyle changes are more likely to succeed.

Addressing the Needs of Heart Failure Patients
For adults over the age of 65 in the United States, heart failure is the leading cause of hospitalization, accounting for more than 1 million hospitalizations (primary diagnosis) annually and over $17 billion in Medicare expenditures.1
Despite significant improvements from medical intervention, over half of patients are readmitted to hospital within one year1. Payers have therefore targeted readmissions as a focus of value-based care initiatives, seeking to both reduce costs and improve quality of care. Today, heart failure readmission rates are publicly reported. Additionally, the Patient Protection and Affordable Care Act imposes financial penalties for the worst performers — hospitals who have the highest readmission rates in the first 30 days after discharge. Hospitals are therefore interested in reducing their readmission rates, leading efforts to:
- Predict patients likely to be readmitted, and;
- Design interventions to prevent readmission.
Effective monitoring of patients after discharge may help the healthcare team recognize early warning signs, enabling them to intervene before emergency readmissions. In order for this to happen, patients must self-monitor and report key biometrics regularly. However, patients don’t often receive effective support in establishing new routines and behaviors after discharge.
Bernard’s Story of Heart Failure and Self-Monitoring
The following is an imagined example showing how, with today’s standard self-monitoring procedures, the typical health journey of a patient with heart failure often ends in hospital readmission within one year of discharge. 1
Emergency department visit and admission
When Bernard experienced unusual shortness of breath that was getting progressively worse, he went to the emergency department and was quickly admitted.
He was soon diagnosed with heart failure. The inside of his heart had experienced an acute backup of blood. Bernard would be forever prone to such events.
This was a shocking and scary time for Bernard and his family.
6.2 million adults in the U.S. live with heart failure. 2

Discharge
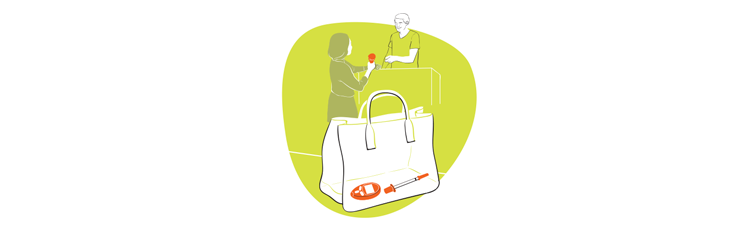
After spending time recovering, it was time for Bernard to go home. Before he could leave hospital, however, Bernard needed to undergo a thorough discharge procedure.
Bernard’s medical team assessed his physical health, cognitive function, and social support, they highlighted all of the medical follow-ups that would be required and introduced him to his new medication regimen.
Bernard’s medical team then explained how important it was for Bernard to self-monitor his symptoms in order to quickly catch warning signs of an impending cardiac event.
From now on, on a daily basis, Bernard would have to track his weight and write his symptoms in a diary.
He was instructed to call the emergency department immediately should he notice any sudden change in his weight.
Bernard’s discharge and education were complete.
As he and his family were leaving the hospital, they reflected on the large amounts of information they had learned and needed to remember.
This was an anxious time for Bernard and his family.
25% of heart failure patients are rehospitalized within thirty days of discharge. Over 61% are rehospitalized within one year. 1

Self-monitoring at home
Bernard was finally at home after a long hospital stay. With the help of his family, Bernard needed to start putting into practice the self-monitoring routine detailed to him by his healthcare team.
This was an exhausting and overwhelming time for Bernard and his family.
While Bernard was initially diligent in self-monitoring his symptoms, he soon disengaged from these activities, not having found a way to integrate them into his daily routine. His family tried to keep him on track but did not always feel confident enough to take on this important responsibility.

Self-monitoring failure and readmission
One month after being discharged from the hospital, Bernard experienced severe swelling in his legs and was readmitted. He had missed signs of increased weight gain, and his heart was backing up again.
Bernard had been unsuccessful in keeping his health stable. Consequently, he was now required to go back and re-live his heart failure journey from the beginning.
- 75% of heart failure readmissions may be preventable. 1
- Heart failure survival is estimated at 46% at five years post-diagnosis and 25% at ten years post-diagnosis.
Identifying Opportunities for Improving the Patient Experience
By examining the failings in Bernard’s self-monitoring experience, we can decipher key lessons that will guide the design of an effective self-monitoring service.
A patient is a human
From hospital admission, to discharge, to subsequent self-monitoring at home, patients and their support networks experience a spectrum of emotions and shifting levels of motivation that make adherence challenging. Simply providing patients with a set of symptom monitoring instructions is unlikely to result in successful uptake and maintenance of self-monitoring behavior over time.
Bridgeable’s approach: Human-centered design
When designing services, Bridgeable takes into account shifting emotional and motivational stages of patients, frontline healthcare providers, caregivers, and other key stakeholders to design effective service elements. An effective self-monitoring service, for example, must work hard to maintain patient compliance by leveraging various patient behaviors and social connections.

The patient journey is complex
The heart failure narrative is not as simple as: ‘The patient is given a self-monitoring tool. The patient self-monitors.’ The experience involves much more. There are multiple settings to consider, education and training requirements, as well as material components involved. There is communication that needs to occur and there is a robust cast of supporting characters, each with roles to play. The details of these elements and the interplay between them must be taken into consideration when designing a service.
Bridgeable’s approach: Leave no stone unturned
At Bridgeable, we look at the patient journey from beginning to end. Along the way, we ask questions that focus on all the issues, from big to small. In fact, we like to work directly with our end users in a co-creative way so that we can better understandall of the important details from their perspective. The answers to these questions guide our design and ensure that a service is set up for success.

The patient is not the only stakeholder
The behaviors, motivations, and barriers experienced by other stakeholders such as healthcare providers and patient support networks must also be considered when designing a self-monitoring service.
Bridgeable’s approach: Adopt a holistic, systemic view
Design elements meant to improve a patient’s experience with a service can create significant positive or negative, cause-and-effect relationships with other components of the system. For a service to be effective, it needs to address the needs of the primary stakeholder — the patient— but also consider others who are impacted, such as caregivers, nurses, and doctors. Relationships and intersections between these stakeholders can reveal opportunities for delivering impact and shared value.

There are no simple solutions, only elegant ones
An effective self-monitoring service must accomplish many objectives. The service must incorporate a robust patient-training component, be able to transmit the patient data to the appropriate parties, allow various parties to communicate with each other, and fit within a hospital’s existing infrastructure, among other key features. An app cannot accomplish this in isolation.
Bridgeable’s approach: Technology is a tool, not a solution
While new technological breakthroughs lead to exciting opportunities for self-monitoring, technology is only a tool that should be used to accomplish specific goals. It should not be used as a substitute for thoughtful service design. A successful service requires technology, people, systems, and communications all working in concert.
Using Service Design to Create Effective Patient Self-Monitoring Services
What does a 21st-century self-monitoring service for complex diseases look like? Future services must address the wide range of needs, capabilities, and motivations of patients, while being flexible enough to integrate within the infrastructure of a patient’s entire care network.
Imagining a SMART self-monitoring service for Bernard

Emergency department visit and admission
Bernard’s story begins the same as before. Bernard is admitted to the hospital for unusual shortness of breath, and is diagnosed with heart failure.

Discharge with SMART service
During discharge, just as before, Bernard is introduced to all of the changes he will need to make in his life. This time, however, Bernard doesn’t have to face this challenge alone. As part of his discharge procedure, Bernard’s nurse introduces him to SMART, the Self-Monitoring Active Response Technology service.
By joining the SMART service, Bernard will be placed under the watchful eye of a Patient Navigator assigned to him. The Patient Navigator will help Bernard incorporate symptom self-monitoring into his routine.
Bernard signs up for the service by completing the consent form and filling out a service customization questionnaire.
Patient Navigator virtual visit
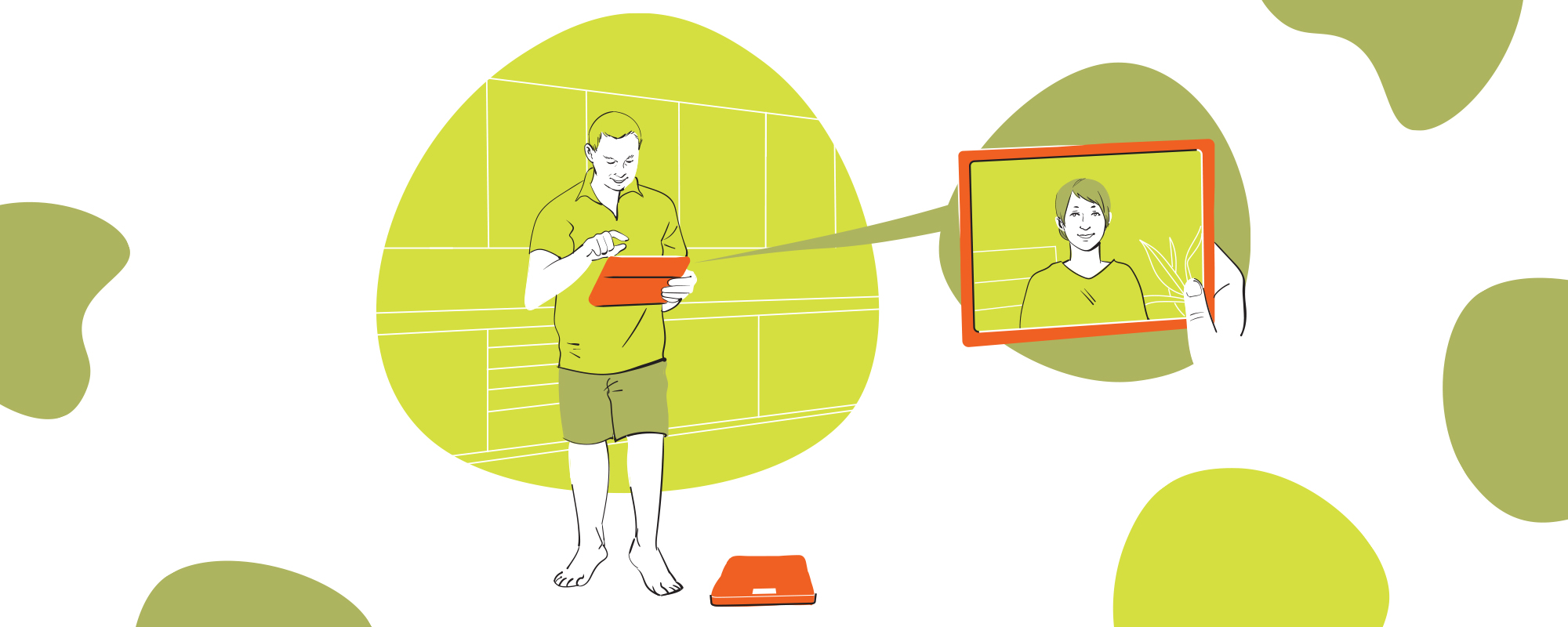
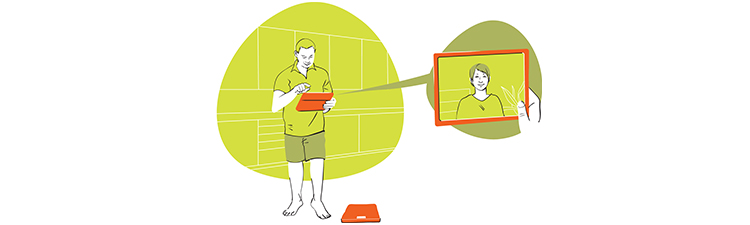
A few days following discharge, Bernard has a virtual meeting with his Patient Navigator, Patty, so that he and his wife can learn how to use the SMART service. Patty orients them via videoconference to the SMART scale that Bernard was sent home with at discharge to help him self-monitor his symptoms.
After some discussion, Patty and Bernard decide to place the SMART scale in the kitchen, so that Bernard can easily integrate its use into his already-established daily routine of taking his medications with breakfast.
Patty then shows Bernard and his wife how self-monitoring works with the SMART device. To ensure Bernard fully understands her instructions, Patty then employs the ‘teach back’ method by asking Bernard to demonstrate back to her how to self-monitor using the device.
Finally, because Bernard indicated in the enrollment questionnaire that he was interested in keeping track of all his data, Patty demonstrates how Bernard and his wife can access his self-monitoring data on a computer, tablet or smartphone.
Self-monitoring at home with Patient Navigator
Every morning during breakfast, Bernard steps onto his SMART scale to measure his weight, which automatically transmits to the SMART service database, giving Patty access to Bernard’s data.
While he weighs himself, Bernard’s SMART scale prompts him to answer a few questions, such as how fatigued he has been in the last 24 hours on a scale of one to ten.

If a self-monitoring check-in is missed
A few weeks into his SMART self-monitoring routine, Bernard finds himself busy helping his son move. Consequently, he forgets to self-monitor. In response to his omission, Bernard receives multiple consecutive warnings from the SMART service. First, Bernard receives an auditory warning from his SMART scale. This is accompanied by a phone notification. When Bernard ignores these warnings, his wife and son receive phone notifications to contact Bernard. After another day of Bernard ignoring these prompts, he receives a call from Patty, who reminds him of the importance of his self-monitoring duties.
With sufficient reminders and his routine returning to normal, Bernard re-initiates his self-monitoring habits.

If a dangerous symptom is detected
A few months later, Bernard’s SMART scale warns him that his weight has increased by three pounds in a single day. This is a cause for concern, and Bernard should seek medical guidance. This advice is emphasized to Bernard when he receives reminders from his wife, his son, and Patty, who have all been notified by the SMART service of Bernard’s concerning symptom.
Bernard calls his doctor who promptly adjusts his diuretic prescription. With this change to his medication, Bernard’s health stabilizes and he avoids hospital readmission.
SMART service graduation
Five months into his SMART self-monitoring routine, Bernard receives a notification from his SMART scale. It tells him that he will be graduating from the full SMART service at the six-month mark, and will no longer need to have Patty watching over him.
With two weeks to go before graduation, Bernard receives a personalized email from Patty. It explains the details of how his self-monitoring routine will change. While Patty will no longer be available to help him, Bernard can keep the SMART scale and continue to use the automated features of the service, if he so desires.
Self-monitoring at home without Patient Navigator
Following his graduation, Bernard continues his daily self-monitoring. He finds it relatively easy now that he has incorporated it into his normal routine. With better control over his health, Bernard continues to enjoy a busy, social, and autonomous life.
References
1 — Parizo, J.T., Kohsaka, S., Sandhu, A.T., Patel, J., Heidenreich, P.A. (2020). Trends in Readmission and Mortality Rates Following Heart Failure Hospitalization in the Veterans Affairs Health Care System from 2007 to 2017. JAMA Cardiology, 5(9)1042-1047.
2 — Virani, S.S., Alonso, A., Benjamin, E.J., Bittencourt, M.S., Callaway, C.W., Carson, A.P., et al. (2020). Heart Disease and Stroke Statistics — 2020 Update: A Report from the American Heart Association. Circulation, 141(9), e139-596.
3 — Taylor C.J., Ordóñez-Mena, J.M., Roalfe, A.K., Lay-Flurrie, S., Jones, N.R., Marshall, T. et al. (2019). Trends in Survival After a Diagnosis of Heart Failure in the United Kingdom 2000-2017: Population Based Cohort Study. BMJ, 364, l223.