
Ideas by Sydney Cooling-Sturges
Building Bridges: Taking small steps toward Value-Based Healthcare
Author

- Sydney Cooling-Sturges
- Senior Service Designer
A value-based healthcare model is a framework for structuring healthcare systems and new delivery models around what matters most to patients – the overall patient experience, the cost to receive care, and, most importantly, the patients’ health outcomes.
The benefits of a value-based healthcare model are clear when it comes to those receiving care, but what about the health systems and caregivers?
Our current fee-for-service healthcare model is volume-driven, meaning healthcare providers see value in serving large volumes of care, but that volume can fluctuate. With staffing shortages and an aging population, that volume can become unsustainable and result in overworked caregivers and poorer patient outcomes, creating a cycle where patients re-enter the health system after receiving care, or are rehospitalized, greatly straining healthcare resources.
A world where patients can expect better health outcomes, and where costs are better managed is not so far away. Whether your goals are to improve utilization of hospital resources or to improve patient outcomes and experiences, implementing components of value-based healthcare helps improve healthcare value for all, not just the patient receiving care.
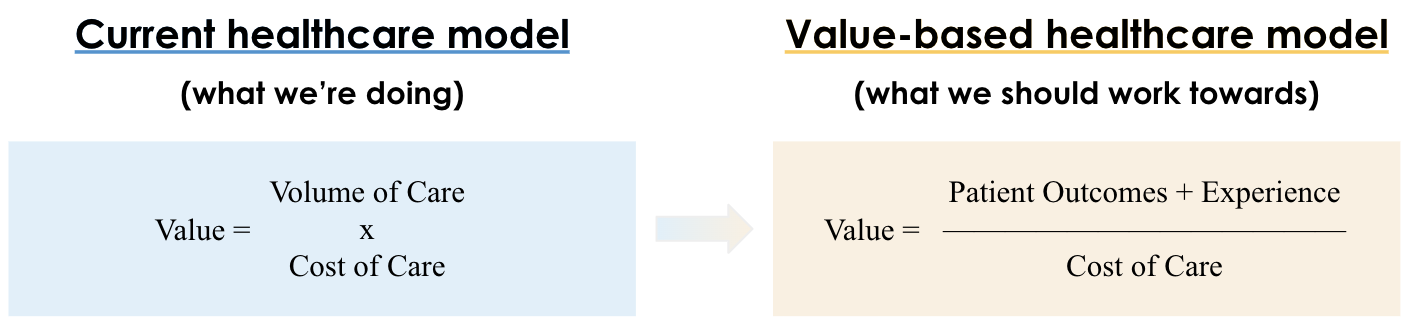
FIGURE 1 – How value is measured in our current healthcare system and the value-based alternative. Currently, value equals volume of care multiplied by cost of care; with value-based, value equals patient outcomes and experience divided by the cost to achieve these outcomes.
Building a new healthcare model
Healthcare systems are increasingly complex, making structural problems difficult to recognize, much less overcome.
When broken down into a few elements, the mutually reinforcing components that perpetuate low-value care become clear. Michael Porter, credited as one of the originators of the term “value-based healthcare” along with Dr. Elizabeth Teisberg in their 2006 book Redefining Healthcare, outlined some of these mutually reinforcing elements and offered alternatives1. While seemingly complex, building towards value-based healthcare is really just taking small steps to offering high-value alternatives to our current, low-value healthcare practices. It’s about countering some of the negative components with positive alternatives, which become easier when we understand the patient perspective.
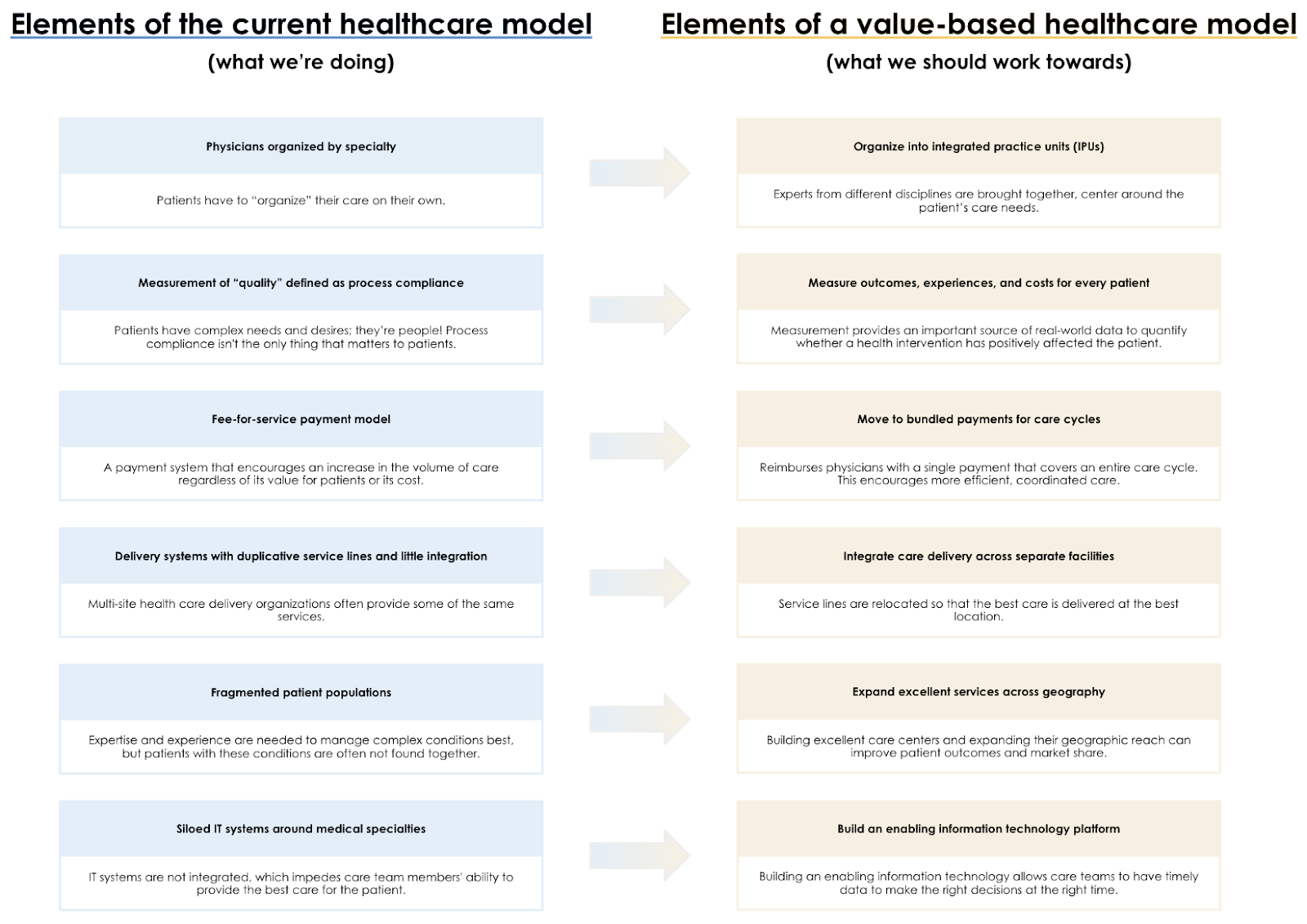
FIGURE 2 – 6 elements of our current healthcare model and their 6 alternative, value-based methods. 1) Physicians organized by specialty; organize into practice units. 2) Measurement of “quality” defined as process compliance; measure outcomes, experiences, and costs for every patient. 3) Fee-for-service payment model; bundled payments for care cycles. 4) Delivery systems with duplicative service lines and little integration; integrate care delivery across separate facilities. 5) Fragmented patient populations; expand excellent services across geography. 6) Siloed IT systems around medical specialties; build an enabling information technology platform.
When faced with a daunting set of barriers, many professionals feel overwhelmed by the sheer size of the task at hand. The magic in value-based healthcare is that it’s a system of initiatives that can be implemented over any length of time, slowly growing momentum and buy-in as implementation progresses.
Each component of the value agenda is distinct, but it’s mutually reinforcing too. An enabling IT platform helps make the measurement of costs, experiences, and outcomes more available. Better measurement of outcomes and costs can help inform bundled payment agreements. Bundled payments give Integrated Practice Units (IPUs) even more incentive to work as a team to improve the value of care. Value continues to rise and costs continue to fall; a negative reinforcing cycle becomes a positive one, just from getting started.
Why now?
Healthcare systems globally are facing key challenges where value-based healthcare could offer potential solutions.
Fee-for-service is unsustainable
The COVID-19 pandemic revealed that our current payment model is not a resilient payment strategy. Fee-for-service is a volume-driven payment system, so when patient volumes dropped in the early stages of the pandemic, especially for elective and primary care, payments decreased substantially2. Providers are recognizing the need to move toward more value-based approaches to payment, such as bundled payments, for more flexibility and protection against future volume shocks.
Enormous staffing shortages
The COVID-19 pandemic also worsened a national shortage of registered nurses both in the United States and Canada, making it increasingly urgent that healthcare organizations undergo a major transformation to focus on retention. Moving to bundled payments and integrating a more enabling IT platform are key tenets of value-based healthcare delivery, and doing so could reduce the time HCPs are spending on administrative tasks and reallocate it to more patient care. When nurses can spend more time with each resident during a shift, not only do outcomes improve, but nursing staff are less likely to experience burnout from overwhelming numbers of patient readmissions.
Aging Populations
In 2021, according to the U.S. Census Bureau, over 16.8% of the U.S. population was aged 65 and older3. That’s 55 million adults with increasing healthcare needs. By 2050, it’s estimated that the number of adults over the age of 65 in the U.S. will reach 90 million. Healthcare expenditure is already growing at more than twice the rate of GDP in the United States¹, and this number will continue to grow as our population continues to age. Shifting toward a value system that incentivizes producing good outcomes that matter to patients will be integral to optimizing costs and providing greater patient benefits.
Policy Changes
Finally, there has been an increased focus on health equity in North America. At the end of 2021, the Centers for Medicare & Medicaid Services (CMS) Innovation Center released a strategy refresh to “transform its delivery system, focus on equity, pay for healthcare based on value to the patient instead of volume of services provided, and deliver person-centered care that meets people where they are.”4 CMS also wants to move 100% of Medicare providers to value-based reimbursements by 2025. Even if Medicare reaches less than the targeted 100% participation by 2025, there is no doubt that value-based healthcare is here to stay.
The adoption of value-based healthcare will continue to accelerate due to these various healthcare challenges and trends, but getting started can feel like a challenge in and of itself – “What if the cost to implement components of value-based healthcare doesn’t pay off?” That’s always a risk with innovation, but consider that there’s a risk with not starting: from continuing to lose money on the inefficient structuring of healthcare today; but also from losing out on the potential savings, increased volume, and improved reputation that a value-based practice could provide.
Value-based healthcare in practice
Incremental changes toward value-based healthcare have shown excellent results all over the world. Below are just a few examples of American healthcare organizations embracing the value-based healthcare agenda to drive down healthcare costs and improve patient outcomes.
- Impact of Organizing Into Integrated Practice Units at Virginia Mason Medical Center
When data showed that Virginia Mason was more expensive than its major competitors, it risked being excluded from a network of high-value hospitals – a major financial and reputational blow for the clinic. Doctors at the clinic determined that collaboration among providers, employers, and health plans was needed to eliminate waste and to provide value-added care only.
One step toward aligning their practice with the interests of patients and payers involved organizing into Integrated Practice Units. These IPUs pair a physical therapist and physician together to standardize their approach to care for patients with common conditions. In doing so, Virginia Mason was able to bring down its use of MRIs – an expensive, low-value test – to diagnose lower back pain and replace it with high-value physical therapy sessions, ordering an MRI in 8% of cases compared to the regional average of 43%. By reducing the use of inefficient and high-cost interventions, the clinic achieved 91% patient satisfaction and could provide same-day appointments in 95% of cases. Virginia Mason demonstrates that improving quality and reducing costs are not mutually exclusive through its use of IPUs.
- Impact of Measuring Outcomes for Every Patient at Cleveland Clinic
The Cleveland Clinic recognized that depressed individuals are at higher risk of cardiovascular disease, hypertension, and diabetes. Patients may feel uncomfortable discussing depression with their doctors, and physicians may not have enough time or skills to determine if a patient is depressed.
To combat this, the Cleveland Clinic began screening every patient over age 12 with a depression screening questionnaire. By screening people, primary care teams could intervene when necessary, which improved people’s questionnaire scores and decreased emergency department use for those patients. Not only does this potentially save lives, but these interventions represent over $1.3 million in savings via prevented ER visits.
-
Medicare’s Bundled Payments for Care Improvement Advanced (BPCIA) program was launched in 2016 to incentivize high-value care. HPMC was accepted into the first cohort of hospitals to participate in the BPCIA program. In this program, Medicare sets a “target price” for an episode of care. If the cost of care for HPMC patients was below the target price, they received a “reconciliation payment” from CMS for the cost savings.
HPMC engaged all stakeholders – patients, hospital staff, physicians, and post-acute facilities – to develop and deliver effective care in the three cardiac and four medical and critical care bundles it participated in under the BPCIA. This led to their use of cost-tracking technology (measurement) and the development of a Continuing Care Team (an integrated practice unit) for patients diagnosed with sepsis.
The results were striking! HPMC reduced its 90-day post-discharge mortality rate for patients in those bundles by 9%. For patients diagnosed with sepsis, HPMC achieved cost reductions 14% below the target price that CMS had set, which projects to $3 million in reconciliation payment.
The counterintuitive truth of value-based healthcare is proven in these examples; the pathway to improving the outcomes and experiences of patients can be the same pathway to reducing costs. What’s more, each of these examples saw great results without implementing every component of value-based healthcare.
Taking the first step
The benefits are clear; Increasing value for patients increases value for everyone. The value agenda works, even when only a few of its components are implemented.
With benefits also comes challenges; Achieving value-based healthcare is difficult. Improving outcomes that matter to patients and optimizing costs requires nothing less than a radical change to our existing systems. Even when the ambition is only to implement one area of value-based healthcare, the transition still can’t be achieved overnight. So, how do you start to implement value-based healthcare? Strategically, iteratively, and collaboratively.
-
Start by defining the problem
Charting a path to value-based healthcare starts with defining the problem. What challenges are happening in your healthcare organization? What components of value-based healthcare could help improve those challenges?
From here, you can identify necessary stakeholders for an initial discussion and identify metrics that will help everyone know when success has been achieved. At Bridgeable, we often say when people are involved with building the bridge, they’re more likely to cross it! Value-based healthcare is all about aligning healthcare with what matters to patients, so identifying and bringing in key patient stakeholders early and often is key to understanding and providing them with what they need. Once the goals of patients are understood, be sure to go back and ensure organizational KPIs are aligned with your patient’s needs and goals.
-
Exploring the problem space
This is where you research, map, build, and design with stakeholders to sort the complexities of the problem and find new areas to explore. What is enabling value-based healthcare in your organization? What isn’t? This is where you learn how hard the effort will be and where you’ll find beautifully easy moments that can help now.
-
Ideating the solution
This is where we discover what we should do and how we should do it through our insights from Step 2. For value-based healthcare, this step may determine what areas of a care pathway, IT system, or patient measurement system should be revised or built toward solving your initial problem and achieving your goals.
-
Build out and pilot the solution
Based on everything discovered in the previous steps, we can start to build and pilot the solution. This is also an area where we can measure the success of our pilot, referring to our KPIs from Step 1.
-
Change management
Value-based healthcare is collaborative and iterative by design, so rolling out, scaling, and iterating your care delivery system is all part of the process. This may involve starting the implementation process over again in a new problem area, building on what you’ve learned from your first pilot to solve problems across your organization!
Great services are not accidental or a stroke of luck – great services are designed – and that means they can be redesigned when necessary. Value-based healthcare presents us with a chance to redesign healthcare services to produce more value for everyone involved.
The transformation to value-based healthcare is neither a quick nor easy process, but it’s certainly worthwhile. We don’t have to start big – we have to understand where we’re headed and work on incremental steps to get there.
A special thank you to Rachel Saks, MSS, LSW, OSW-C, Senior Director, Education at Cancer Support Community and Elliott Wortham, Health & Well-Being Service Designer, whom we had the pleasure of speaking with to better understand the benefits of value-based healthcare and the barriers to getting started.
References
1 —Porter, M & Lee, T. The Strategy That Will Fix Health Care. Harvard Business Review. 2013 October. https://hbr.org/2013/10/the-strategy-that-will-fix-health-care
2 —Glauser W. Pandemic amplifies calls for alternative payment models. CMAJ. 2020 Jun 8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7867211/
3 —American Community Survey. S0103 POPULATION 65 YEARS AND OVER IN THE UNITED STATES. United States Census Bureau. 2021. https://data.census.gov/cedsci/table?q=s0103
4 —Strategic Direction, Background on the CMS Innovation Center 2021 Strategy Refresh – Putting All Patients at the Center of Care. Centers for Medicare & Medicaid Services. 2021. https://innovation.cms.gov/strategic-direction